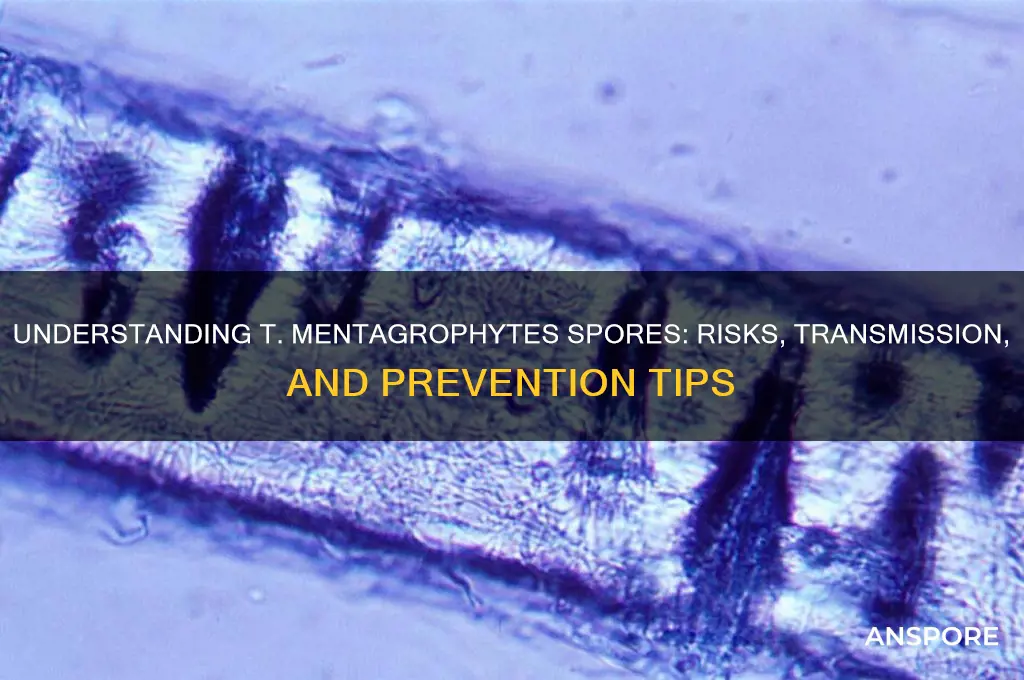
*Trichophyton mentagrophytes* is a dermatophyte fungus commonly associated with skin, hair, and nail infections in humans and animals. Its spores, known as conidia, play a crucial role in its lifecycle and transmission. Understanding the nature of *T. mentagrophytes* spores is essential for diagnosing and managing infections, as they are highly resilient and can survive in various environments, contributing to the spread of conditions like ringworm, athlete’s foot, and nail fungus. Research into their structure, dispersal mechanisms, and resistance to environmental factors is vital for developing effective antifungal treatments and preventive strategies.
What You'll Learn
- Spores Structure: Morphology, size, shape, and unique features of T. mentagrophytes spores under microscopy
- Spores Transmission: Modes of spore spread, including direct contact, fomites, and environmental surfaces
- Spores Survival: Environmental conditions affecting spore longevity, such as humidity, temperature, and surfaces
- Spores Infection: Role of spores in initiating dermatophytosis and their interaction with human skin
- Spores Detection: Laboratory methods for identifying T. mentagrophytes spores, including culture and PCR techniques

Spores Structure: Morphology, size, shape, and unique features of T. mentagrophytes spores under microscopy
Under microscopy, *Trichophyton mentagrophytes* spores, known as macroconidia, reveal a distinct morphology that aids in their identification. These spores are typically hyaline (colorless) and exhibit a cylindrical to slightly clavate (club-shaped) structure. Their size ranges from 4 to 8 μm in width and 8 to 50 μm in length, making them larger than the microconidia produced by the same fungus. This size variability is a key feature for differentiation under microscopic examination. The walls of the macroconidia are smooth and thin, contributing to their translucent appearance. These structural characteristics are essential for mycologists and clinicians in diagnosing dermatophytosis caused by *T. mentagrophytes*.
The shape of *T. mentagrophytes* macroconidia is another critical identifier. They are often described as having a slightly tapered or rounded apex, with a base that may be truncate or slightly rounded. The spores are typically multicellular, with septa (cross-walls) dividing them into multiple compartments. This multicellular nature distinguishes them from the unicellular microconidia. The arrangement of these septa can vary, but they are generally evenly spaced, contributing to the spore’s overall symmetry. Understanding these shape nuances is vital for accurate microscopic identification, especially when distinguishing *T. mentagrophytes* from closely related species like *Trichophyton interdigitale*.
One of the most unique features of *T. mentagrophytes* spores is their ability to retain their shape and structure even after prolonged exposure to environmental stressors. This resilience is attributed to their robust cell wall composition, which includes chitin and glucan layers. Under microscopy, this durability is evident in the spores’ consistent morphology across different samples and conditions. Additionally, the spores often exhibit a slight curvature, which can be more pronounced in older cultures. This curvature, combined with their size and septation, creates a distinctive profile that aids in their identification even in mixed fungal cultures.
For practical purposes, examining *T. mentagrophytes* spores under a 40x to 100x magnification is recommended to observe their detailed morphology. Using a lactophenol cotton blue stain can enhance contrast, making the cell walls and septa more visible. Clinicians and laboratory technicians should pay particular attention to the size range and septation patterns, as these are the most reliable features for identification. While automated systems like MALDI-TOF mass spectrometry are increasingly used for fungal identification, microscopy remains a cost-effective and accessible method for initial diagnosis. Mastering the unique features of *T. mentagrophytes* spores under microscopy ensures accurate and timely treatment of dermatophyte infections.
Are Space Spores Real? Exploring the Science Behind Cosmic Microbes
You may want to see also

Spores Transmission: Modes of spore spread, including direct contact, fomites, and environmental surfaces
Direct contact remains the most straightforward yet often overlooked mode of spore transmission. When an individual touches an infected person or animal, *T. mentagrophyte* spores can transfer directly to the skin, nails, or hair. This is particularly common in households with pets, as animals like cats and dogs can harbor the fungus without showing symptoms. For instance, petting an infected cat and then scratching your scalp can introduce spores to your skin, potentially leading to ringworm. To mitigate this, wear gloves when handling pets with suspected infections and wash hands thoroughly with soap and water after contact. Children, who often engage in close play with pets, are especially vulnerable, so parental supervision and hygiene education are critical.
Fomites—inanimate objects capable of carrying infectious agents—play a silent but significant role in spore spread. *T. mentagrophyte* spores can survive on surfaces like combs, brushes, towels, and clothing for weeks, waiting for a new host. Gyms, schools, and shared living spaces are high-risk environments due to communal items. For example, borrowing a friend’s hairbrush or wearing unwashed gym clothes can expose you to spores. Disinfecting shared items with antifungal solutions (e.g., diluted chlorine bleach or specialized fungicides) and avoiding the sharing of personal care items are practical steps to break this transmission chain. Regular laundering of clothing and bedding in hot water (60°C or higher) can also kill spores effectively.
Environmental surfaces act as reservoirs for *T. mentagrophyte* spores, particularly in damp, warm conditions. Soil, carpeting, and shower floors are common habitats where spores thrive. Walking barefoot in contaminated areas, such as locker room floors or gardens, can lead to infection, especially if the skin is compromised (e.g., through cuts or scratches). Public spaces like swimming pools and saunas are also potential hotspots. To reduce risk, wear flip-flops in communal areas, keep living spaces dry and well-ventilated, and vacuum carpets regularly, disposing of the vacuum bag immediately to prevent spore recirculation. For outdoor activities, consider wearing gloves when gardening and washing hands promptly afterward.
Understanding the interplay of these transmission modes is key to prevention. While direct contact and fomites often dominate discussions, environmental surfaces contribute to long-term spore persistence. For instance, a child playing in a spore-contaminated sandbox might transfer spores to their hands, then to a shared toy (fomite), and finally to a sibling through direct contact. Breaking this cycle requires a multi-pronged approach: personal hygiene, environmental sanitation, and awareness of high-risk settings. Schools and daycare centers should implement regular cleaning protocols, especially for shared toys and play areas, to protect young children, who are more susceptible due to developing immune systems and frequent close contact.
In high-risk populations, such as immunocompromised individuals or those with frequent exposure (e.g., veterinarians), proactive measures are essential. Regular skin inspections, antifungal powders in shoes and socks, and barrier creams can provide additional protection. For those already infected, isolating contaminated items and treating pets simultaneously are crucial to prevent reinfection. While *T. mentagrophyte* spores are resilient, consistent adherence to these strategies can significantly reduce transmission, turning a pervasive problem into a manageable one.
Exploring Spore's Gameplay Length: How Long Does the Adventure Last?
You may want to see also

Spores Survival: Environmental conditions affecting spore longevity, such as humidity, temperature, and surfaces
Spores of *Trichophyton mentagrophytes*, a fungus responsible for ringworm and other dermatophytoses, are remarkably resilient, capable of surviving in diverse environments for extended periods. Their longevity hinges on a delicate interplay of environmental factors, primarily humidity, temperature, and the surfaces they inhabit. Understanding these conditions is crucial for devising effective strategies to control their spread.
Humidity: The Lifeline of Spores
High humidity levels are a spore’s best friend. *T. mentagrophytes* spores thrive in environments with relative humidity above 60%, as moisture facilitates their adhesion to surfaces and delays desiccation. In contrast, dry conditions below 40% can significantly reduce spore viability within days. For instance, spores on a damp bathroom floor may persist for months, while those on a dry, sunlit windowsill could become inert within weeks. Practical tip: Maintain indoor humidity below 50% using dehumidifiers to discourage spore survival, especially in areas prone to fungal growth.
Temperature: The Double-Edged Sword
Temperature plays a dual role in spore longevity. *T. mentagrophytes* spores exhibit optimal survival at temperatures between 20°C and 30°C (68°F–86°F), mirroring their preference for warm-blooded hosts. However, they can endure extremes, tolerating temperatures as low as 4°C (39°F) and as high as 50°C (122°F) for short periods. Prolonged exposure to temperatures above 60°C (140°F) or below 0°C (32°F) effectively kills spores. Caution: Avoid relying solely on temperature extremes for eradication, as spores can revive when conditions become favorable again.
Surfaces: The Silent Carriers
The type of surface a spore lands on profoundly impacts its survival. Porous materials like fabric, wood, and soil provide crevices where spores can embed and evade cleaning efforts, surviving for years. Non-porous surfaces like glass, metal, and plastic are less hospitable but still pose risks if not regularly disinfected. For example, spores on a gym mat can persist for months, while those on a stainless steel doorknob may last only days. Instruction: Use antifungal agents containing benzalkonium chloride or iodine to disinfect surfaces, ensuring thorough coverage to dislodge embedded spores.
Practical Takeaway: A Holistic Approach
Controlling *T. mentagrophytes* spores requires a multifaceted strategy. Reduce humidity, regulate temperature, and prioritize surface disinfection to disrupt their survival mechanisms. For high-risk areas like gyms or pet environments, implement routine cleaning protocols and educate individuals on preventive measures, such as wearing protective footwear in communal spaces. By manipulating these environmental conditions, you can significantly curtail spore longevity and mitigate the risk of infection.
Are Angiosperm Eggs Spores? Unraveling Plant Reproduction Mysteries
You may want to see also

Spores Infection: Role of spores in initiating dermatophytosis and their interaction with human skin
Spores of *Trichophyton mentagrophytes* are resilient, dormant structures that serve as the primary agents of dermatophytosis transmission. These spores, known as arthroconidia, can survive for months in environments like soil, animal fur, or even gym floors, waiting for an opportune host. Unlike active fungal cells, spores are metabolically inactive, making them resistant to desiccation, temperature fluctuations, and many disinfectants. This durability ensures their longevity and increases the likelihood of encountering human skin, the gateway to infection. Once in contact with a suitable environment—warm, moist, and nutrient-rich—these spores germinate, initiating the fungal invasion that characterizes dermatophytosis.
The interaction between *T. mentagrophytes* spores and human skin is a complex, multi-step process that hinges on adhesion and penetration. Spores first attach to the stratum corneum, the outermost layer of the epidermis, using surface proteins and adhesins. This adhesion is facilitated by the skin’s natural moisture and slight alkalinity, which activate the spores. Next, the spores secrete keratinases, enzymes that degrade keratin, the primary protein in skin, hair, and nails. This enzymatic activity weakens the skin barrier, allowing hyphae—the filamentous form of the fungus—to penetrate deeper layers. For individuals with compromised skin integrity (e.g., cuts, eczema, or excessive sweating), this process is expedited, increasing infection risk.
Preventing spore-induced dermatophytosis requires a two-pronged approach: environmental control and personal hygiene. In high-risk settings like locker rooms or farms, regular cleaning with fungicidal agents (e.g., chlorine or quaternary ammonium compounds) is essential to eliminate spores from surfaces. For personal protection, wearing protective footwear in communal areas and avoiding direct contact with potentially contaminated animals (e.g., cats, dogs, or cattle) is critical. After exposure, thorough handwashing and skin drying can remove spores before they germinate. For those with recurrent infections, antifungal powders containing miconazole or clotrimazole (applied twice daily for 2–4 weeks) can create an inhospitable environment for spore activation.
Treatment of established dermatophytosis caused by *T. mentagrophytes* spores often involves both topical and systemic antifungals, tailored to the infection’s severity and location. Mild cases, such as tinea corporis (ringworm), typically respond to topical terbinafine cream (1–2 applications daily for 2–4 weeks). However, deeper infections like tinea capitis (scalp ringworm) or onychomycosis (nail fungus) may require oral terbinafine (250 mg daily for 6–12 weeks) or itraconazole (200 mg daily for 4–8 weeks). It’s crucial to complete the full course of treatment, as premature discontinuation can lead to recurrence. Additionally, combining treatment with spore prevention strategies minimizes the risk of reinfection, ensuring long-term resolution.
Understanding the role of *T. mentagrophytes* spores in dermatophytosis highlights the importance of early detection and proactive management. Spores are silent carriers of infection, often asymptomatic until they germinate and colonize. Regular skin inspections, especially for individuals in high-risk groups (e.g., athletes, farmers, or pet owners), can catch infections before they spread. For households with infected pets, concurrent veterinary treatment and environmental decontamination are non-negotiable. By targeting spores at every stage—from environmental persistence to skin interaction—we can disrupt the cycle of dermatophytosis and protect both human and animal health.
Mastering Spore: A Step-by-Step Guide to Activating Cheats Easily
You may want to see also

Spores Detection: Laboratory methods for identifying T. mentagrophytes spores, including culture and PCR techniques
Observation: *Trichophyton mentagrophytes* is a dermatophyte fungus responsible for ringworm infections in humans and animals, and its spores are key to diagnosis and treatment. Detecting these spores in clinical samples requires precise laboratory methods to differentiate them from other fungi. Two primary techniques—culture and PCR—offer distinct advantages and limitations, making them complementary tools in mycological diagnostics.
Analytical Approach: Culture-based methods remain the gold standard for identifying *T. mentagrophytes* spores. Samples are inoculated onto Sabouraud dextrose agar or dermatophyte test medium (DTM), where the fungus grows into characteristic colonies within 7–14 days. DTM, in particular, includes phenol red as a pH indicator, turning colonies red due to urease activity, a hallmark of *T. mentagrophytes*. Microscopic examination of slide cultures reveals macroconidia (large, thick-walled spores) with a distinctive "brick-like" appearance. However, culture methods are time-consuming and may yield false negatives if spores are non-viable or present in low quantities.
Instructive Steps: PCR techniques provide a faster, more sensitive alternative for spore detection. DNA extraction from clinical samples is followed by amplification of species-specific gene targets, such as the internal transcribed spacer (ITS) region or the 28S ribosomal RNA gene. Primers designed for *T. mentagrophytes* ensure specificity, and results are available within hours. For instance, a nested PCR assay targeting the ITS1 region can detect as few as 10 spores per sample. Caution must be taken to prevent contamination, as PCR is highly sensitive to false positives. This method is particularly useful for confirming culture results or identifying spores in non-viable samples.
Comparative Analysis: While culture methods offer morphological confirmation and antibiotic susceptibility testing, PCR provides rapid, unambiguous identification. Culture is cost-effective and widely accessible but lacks sensitivity for low-spore samples. PCR, though more expensive and technically demanding, is ideal for urgent cases or mixed infections. Combining both methods enhances diagnostic accuracy, especially in complex clinical scenarios. For example, a study comparing the two techniques found PCR detected *T. mentagrophytes* in 95% of cases, while culture identified 78%, with 70% concordance between methods.
Practical Takeaway: Laboratories should tailor their approach based on sample type, turnaround time, and resources. For routine dermatophyte identification, culture remains reliable, but PCR is invaluable for challenging cases or epidemiological studies. Clinicians should provide detailed patient history and sample collection instructions to optimize results. For instance, hair samples should be plucked at the base to include the spore-rich hair shaft, while skin scrapings must be taken from active lesion margins. Proper sample handling and method selection ensure accurate detection of *T. mentagrophytes* spores, guiding effective antifungal therapy.
Unveiling the Fascinating World of Fern Spores: How They Work
You may want to see also
Frequently asked questions
T. mentagrophytes, or Trichophyton mentagrophytes, is a species of fungus that belongs to the dermatophyte group. It is commonly associated with skin, hair, and nail infections in humans and animals.
Yes, T. mentagrophytes produces spores, specifically arthroconidia, which are asexual spores that play a key role in its transmission and survival in the environment.
T. mentagrophytes spores can be transmitted through direct contact with infected individuals, animals (e.g., pets), or contaminated objects like clothing, towels, or surfaces.
Yes, T. mentagrophytes spores are highly resilient and can survive in the environment for extended periods, making them a persistent source of infection.
T. mentagrophytes spores can be eliminated using antifungal agents, thorough cleaning of contaminated surfaces, and proper hygiene practices to prevent their spread.